Is Pain Worse After Nerve Blocks? 6 Factors to Know About Nerve Blocks

People may feel some hesitation when it comes to trying nerve blocks to help with pain management. Will it possibly make your pain worse after nerve blocks are administered?
If you are suffering from pain, then you are likely willing to try any safe procedures to try and eliminate that pain. Whether your pain is from an injury, an autoimmune disorder, arthritis or some nerve related issue, finding a resolution is a priority.
Working with your pain management specialist, you may create a treatment plan that involves nerve blocking. This procedure can have dual uses:
- One is to identify the source of the nerve pain
- The other is to alleviate the nerve pain
Nerve blocks can also be used to help eliminate causes of pain. For instance, if your doctor numbs nerve endings but your pain persists, you can know that area is not the source of your pain.
What Are Nerve Blocks?
These injections have been found to help many people have more functioning and higher quality of life. Many, before receiving injections, are afraid the pain will be worse after nerve blocks. The answer to this question is complex and depends on many individualized factors.
However, for most, they offer pain relief that other treatment methods have been unable to do.
Keep reading to learn 6 factors about nerve blocks, including if pain is worse post-nerve block procedure.
1. Different Types of Nerve Blocks
There are several nerve block procedures, each with a specific goal, to offer you pain relief. However, they do so in different ways:
- Selective nerve root injections are used to reduce inflammation of the spinal nerve. An injection is made at the root of the nerve to deaden the nerves following that path.
- Radial nerve blocks focus on treating nerves in the hand and arm.
- Femoral nerves run from the spine all the way down your legs.
- Femoral nerve blocks go into the groin area to treat the area causing irritation.
These blocks are done with guided ultrasound equipment, making it quick and simple for doctors to complete the procedures.
In addition:
- Local nerve blocks are done by injecting a local anesthetic to a nerve area. Epidurals are good examples of local nerve blocks. They are usually temporary sources of pain relief.
- Neurolytic blocks are used to treat chronic pain symptoms. Your doctor uses alcohol or a freezing agent. This block is not used for ordinary pain relief. Because it causes damage to the nerve pathway, it is typically reserved for more serious conditions.
- Surgical nerve blocks make it possible for surgeons to remove damaged nerves or to allow the doctor to damage specific areas in order to stop pain. This technique has permanent affects and is also reserved for the more serious conditions.
2. Benefits of Nerve Blocks
There is one major benefit of nerve blocks, it relieves pain. It is the painful conditions that can be treated with a nerve block that makes this procedure advantageous.
Nerve blocks can be used during childbirth to alleviate labor and delivery pain without harming the infant. They can be administered after surgeries to get rid of any pain associated with the surgery itself.
Furthermore, nerve blocks can ease:
- Cancer-related pain
- Arthritis
- Lower back pain
- Headaches
- More serious conditions such as chronic regional pain syndrome
Additional conditions treated by nerve blocks include shingles, herniated disks, and remarkably, phantom pain after an amputation.
3. Nerve Block Procedure
Performing a nerve block will usually take less than half an hour. The doctor simply numbs the area where the needle will be inserted. Using an ultrasound, the doctor moves the needle to the site that needs treatment. Once there, anesthetic medication is released.
You will then be allowed to rest for a while before being discharged.
4. Reasons to Get a Nerve Block
Alleviating pain is the main reason to have a nerve block procedure. But there are other things a nerve block can help resolve. For instance, they can help your doctor determine the source of your pain.
If your doctor is providing long-term treatment to you for a serious medical condition, he or she can use a nerve block to determine how anesthetics will respond, how well it will meet your pain-relieving needs.
Nerve blocks are often used during surgeries, both major and minor. Some people feel pain from the incisions made during a surgery. Nerve blocks can help ease this pain. Other surgeries are small and need a brief period of pain relief for the patient. Nerve blocks provide this relief.
Conditions such as cancer are treated with nerve blocks when other medicines are not working. Some pain-relieving agents cause vomiting, nausea and other negative side effects. Some pain medicines just do not work. In these cases, nerve blocks are used.
5. How Long Do Nerve Blocks Last?
The amount of pain relief you receive from a nerve block depends on the type of procedure you had, whether your condition is temporary or chronic, and your own body. As with many other things, nerve block results can vary among individuals.
Most patients report relief for several hours, some report relief for several days. For those with chronic pain conditions, doctors may use nerve blocks that last up to a year. In some cases, doctors can insert a pump that will release anesthetic as needed, based on your needs.
Nerve blocks are made to treat temporary pain. This means that once the nerve block wears off, you should notice a decrease in pain at the original source, and no longer feel the need for the nerve block.
6. Is Pain Worse After Nerve Blocks?
For most, pain after a nerve block fades. Everyone may have a different recovery. Some may feel soreness at the site of the injection, others may experience swelling that can compress the nerves and cause pain for a little while longer. But this pain is temporary.
These symptoms should subside over a short period, allowing you to get back to living a fully functional life.
There are no complete guarantees with nerve blocks. However, feedback regarding the success of nerve blocks is encouraging.
Migratory Arthritis: Causes, Symptoms, and Treatment Options

There are many types of arthritis that people may suffer from, but one of the least well-known is migratory arthritis. To fully understand this condition, we’ll explore the causes, symptoms, and treatment options.
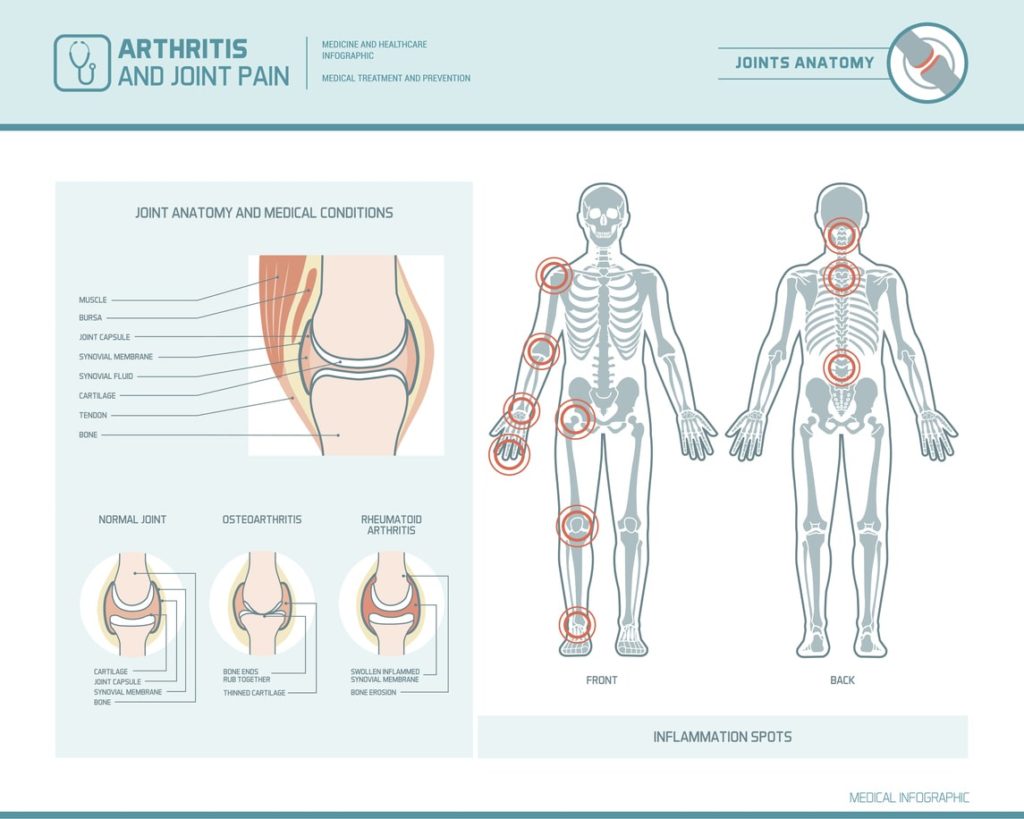
A joint is a point where two or more bones meet. The space between each joint can swell or become inflamed. This is called arthritis and it can be very painful.
Because there are 360 joints in the human body, that is 360 places for arthritis to appear. Unfortunately, pain from arthritis is very common.
According to the Center for Disease Control, by the year 2040, 78 million American adults are expected to be diagnosed with some form of arthritis. This number is concerning since arthritis is a leading cause for disability in the United States.
Just when you think having arthritis pain in one joint is bad enough, researchers have learned that arthritis can travel from one joint to another.
This is called migratory arthritis.
What is Migratory Arthritis?
The word “migratory” suggests movement of some kind. And that is exactly what it means in relation to arthritis.
For instance, the joint in your knee may be inflamed and causing pain. After a while, you may notice that the joint in your ankle is feeling pain also. This can mean your arthritis has migrated, or traveled, from your knee to your ankle.
Your arthritis can spread from one joint to other joints in your body, even if the joint that was initially swollen and inflamed has begun to feel better.
What Causes Migratory Arthritis?
When arthritis spreads, it may be because of an underlying disease or ailment. Inflammatory bowel disease and hepatitis B and C are common causes of this type of arthritis.
In addition, migratory arthritis is most often found in gout, osteoarthritis, and rheumatoid arthritis.
- Gout happens when there is a crystal build-up between the joints.
- Osteoarthritis is a breakdown of cartilage that covers the bones in your joints.
- Rheumatoid arthritis occurs when you body attacks its own healthy tissues
Other Diseases Connected to Pain in Multiple Joints
Other illnesses connected to migratory arthritis include:
- Infectious arthritis
- Lupus
- Lyme’s
- Rheumatic fever
- Whipple’s disease
Infectious arthritis happens when germs enter your body and travel to a joint, and then to another joint, and another. This is like gonococcal arthritis except that the germs in these cases derive from the disease gonorrhea.
Lupus is a form of chronic inflammation in the body. It is an autoimmune disease that affects all major organs and joints. With lupus, your immune system is attacking its own healthy joints. Lupus is getting easier to diagnose but there was a time when it was difficult due to the ability of lupus to appear like other types of arthritis.
Lyme disease is another form of chronic inflammation that leads to migratory arthritis. It is caused by a bacterium carried by deer ticks. When the tick carrying the bacteria bites you, the bacteria then travels throughout your body.
This can also be caused by an injury that has not healed properly.
Symptoms of Migratory Arthritis
There are many common symptoms of this type of arthritis. No matter what the cause, symptoms can be commonly recognized.
1. Pain
Pain is typically the number one symptom associated with migratory arthritis. This, and chronic swelling. Additional symptoms can include redness in the area that is causing pain or that is swollen.
Rashes and fever can accompany arthritis.
2. Weight Changes
One symptom you may not associate with migratory arthritis right away is changes in your weight. Some people have noted losing weight without trying, while others have found it difficult to lose weight.
In fact, they have noted they gained weight even when trying to lose.
3. Fatigue
If you are feeling tired more often than before, this too could be a symptom of this type arthritis. Fatigue is a common symptom with all types of arthritis.
Fatigue is something that begins to interfere with your daily tasks because you do not have the energy to complete them.
4. Joint Stiffness
When one or multiple joints stiffen and it becomes to affect your range of motion, you may be experiencing migratory arthritis. This may even cause you to limp or use your joints differently to avoid the pain.
For instance, if the joint in your right ankle has arthritis, you may try to avoid using that ankle and put more pressure on the ankle without arthritis.
Doing so can change the way you walk.
5. Sadness
Finally, it is important to note that any type of arthritis can affect your mental health as well as your physical health.
If you notice you are having symptoms of sadness, excessive crying, and unmerited anxiety for no reason, it could be due to this arthritis.
After all, if you feel bad in any area of your body, it can become the focus of your thoughts and feelings until you receive treatment.
Migratory Arthritis Treatment
Receiving treatment as early as you can is the best solution for healing any ailment. Unfortunately, it is not always that easy to do, especially with conditions like arthritis that can be misdiagnosed in the beginning stages.
To catch it early, though, start documenting any symptoms you have, whether you think they are meaningful or not, and share this information with your doctor.
These symptoms could be used later to help in diagnosing your pain and developing a treatment plan.
Even if you aren’t documenting, there are great treatments available. Your pain management clinic specialist will be able to assess your needs and offer you the treatment most fitting.
1. Physical Exams
Your doctor will complete a physical exam to check the alignment of your joints, the tenderness of the area surrounding your joints, and your range of motion.
Treatments can include simple over the counter medications that reduce inflammation. Or, doctors may prescribe topical creams and lotions. If those do not work, you can discuss prescription pain medications with your doctor.
2. Steroid Injections
Furthermore, joint injections or medial branch blocks that release a corticosteroid into the joint area has given many people relief from pain.
The first step in getting help is to contact your pain management specialist. Together, you can develop a plan to treat your symptoms and prevent further migrations.
Arthritis Awareness Month: How an Arthritis Treatment Center Can Help

May is Arthritis Awareness Month, so this year, we will discuss the different therapies offered at an arthritis treatment center that may help reduce pain.
According to the Arthritis Foundation, arthritis is the leading cause of disability in America. An estimated 54 million people, including adults and children, have been diagnosed with some form of arthritis. The most common form is osteoarthritis.
The feeling of pain is a signal that tells you something is wrong in your body. Pain from arthritis means there is something wrong in the area of your joints.
Acute vs. Chronic Arthritis
While your body releases its own painkilling chemicals, endorphins, this may not always be enough, depending on if the pain is acute or chronic.
Acute
Acute arthritis pain is temporary, it comes and goes. It can normally be treated with:
- Medication
- Hot and cold wraps
- Other simple therapeutic techniques
Acute pain can last for a few days or a few weeks, but not typically longer than that. Examples are an arthritic flair or gout attack.
Acute arthritis pain feels like sharp, shooting pains.
Chronic
Chronic arthritis pain lasts longer, for at least three months. It can even last years if not treated. Joint pain, migraines, and nerve damage are associated with chronic pain.
Examples include:
- Complex regional pain syndrome
- Fibromyalgia
Chronic arthritis pain feels like dull, throbbing aches and pains.
The good news is that there are treatments that can reduce the pain you feel.
Keep reading to discover methods of relief being used by specialty doctors at an arthritis treatment center.
Beginning Therapies Available at a Arthritis Treatment Center
You may have likely tried to treat your arthritis using the first line of defense for most arthritis sufferers. And they may have given you some relief.
These include analgesics like ibuprofen and naproxen. You may have even tried alternating heat and cold to treat the inflammation.
Another beginning therapy is the continue to exercise. This sounds counter-effective, but it is true that the more you can move your joints, the more your joints will stay flexible. This does not mean you need to participate in hard core aerobic activities.
Taking short walks and stretching can go a long way in treating arthritis.
While exercise is helpful, it may not always solve the problem on its own. Other techniques your arthritis treatment center doctor may want to try includes:
- Joint injections
- Medial branch blocks
- Join replacements
1. Joint Injections
Joint injections are exactly what they sound like, the doctor injects medicine directly into the joints. There is very little risk with this method that can alleviate swelling and pain in the joints.
Joint injections at an arthritis treatment center can help your doctor get a better diagnosis of what is causing your swelling and pain. He or she can analyze your joint fluid.
Doing so helps determine if it is gout, an infection or some other reason for the inflammation.
What gets injected into your joint is usually a simple combination of steroids and something to numb the area.
Depending on the location of the joint, your doctor may choose to use an ultrasound to help guide them to the right point.
Doctors have options when it comes to the type of injections to treat your pain.
– 1. Corticosteriod injections:
Typically, the first choice at an arthritis treatment center is a corticosteroid injection, which last for two or three months.
– 2. Hyaluronic acid injections:
If these don’t work, doctors may choose to use hyaluronic acid injections.
This type of injections is very similar to your natural joint fluid.
There are medical claims that hyaluronic acid coats the nerves and helps your body restore it natural fluids in the area of inflammation. It can last for up to six months.
– 3. Platelet-rich plasma injection:
A third type of joint injection is called platelet-rich plasma injection. These use your own blood and platelets to encourage healing of your arthritis.
Placental tissue matrix injections are also considered. This fourth type of injection is said to be a good pain reliever of pain from arthritis.
After resting and caring for the joint in the first two days after the joint injection, you should be feeling much better and the pain should subside.
Your arthritis treatment center can help you determine which type of injections are right for you.
2. Medial Branch Blocks
Back and neck pain can become unbearable for some. Using medial branch blocks can help ease this pain.
Your spine is lined with facet joints between each vertebra. They help with stability and flexibility. If they become inflamed due to arthritis, you may find it difficult to function.
This is called facet syndrome.
To help ease your pain, your doctor may choose a medial branch block, which involves injecting an anesthetic and steroid agent into the joints affected. This interrupts the sensory nerve that supplies the joint with the feeling of pain.
- Medial branch blocks offer long-term pain relief results.
- They can also help in preparation if further treatment is needed, such as radiofrequency neurotomy, which delivers thermal denervation to the facet joint to relieve pain.
- Simply, thermal energy is used to deaden the nerves supplying the joints with pain signals.
3. Joint Replacements
There are times when all other treatment methods do not help you maintain the quality of life you prefer due to arthritic pain.
You have most likely tried all other techniques and while they may have worked for a while, they are no longer easing your pain.
If this is the case, talk to an arthritis treatment center to see about joint replacements.
In cases such as this, having a joint replacement may be option your pain management specialist will discuss with you.
It is amazing the progress the medical profession has made in treating arthritis. Today, if you have a joint that can no longer be treated, specialists can replace that joint with a plastic or metal prosthesis, allowing you to return to full use of your joints, pain-free.
It is a surgical procedure, but recovery is often quick and with little pain. Most joint replacements are done to knees and hips. However, they can ease pain in other joints as well, including:
- Hands
- Ankles
- Hands
- Elbows
Conclusion
In conclusion, there is relief for the joint pain you may be dealing with today. Finding the right arthritis treatment center is important to receiving the best care for your joint pain.
You do not have to suffer with arthritis pain forever. Reach out and ask for help today.
How to Avoid a Fibromyalgia Misdiagnosis

Those suffering from fibromyalgia suffer from constant pain and a fibromyalgia misdiagnosis can be detrimental. Here’s what to know about a diagnoses of fibromyalgia.
Pain, fatigue, sleep problems, inability to concentrate, numbness, headaches, and digestive problems. These are just a few of the first signs of fibromyalgia that doctors see when trying to assist patients.
According to the National Fibromyalgia Association, 10 million people are affected by this disorder in the United States. Most of these are women and the symptoms can vary from person to person.
Unfortunately, many doctors unknowingly give a patient a fibromyalgia misdiagnosis and are prescribing a one-size fits all treatment plan.
This may be because fibromyalgia is still a mystery. No one has definitively found why it exists and how to cure it.
What is Fibromyalgia?
Fibromyalgia is a syndrome that consists of a group of symptoms that appear together. For example, pain in the joints will be accompanied by headaches, tingling in the legs and trouble sleeping.
Many researchers believe this disorder stems from a brain problem. Meaning, the brain gets confused and misinterprets how to respond to certain factors.
When a person sees a bright light, a normal brain may make a person squint a bit until the eyes can adjust.
In a person with fibromyalgia, the brain sends signals to the body that say the bright light is painful, making the person unable to adjust to the light and even develop other painful symptoms.
A problem arises when doctors mistake the symptoms of their patients and provide a fibromyalgia misdiagnosis, preventing them from proper treatment.
The Misdiagnosis of Fibromyalgia
Today, it seems like fibromyalgia is the go-to diagnosis when no other diagnosis can be made. This can become a problem when establishing a treatment plan.
Some reports claim 2/3 of people given a diagnosis of fibromyalgia are misdiagnosed.
This is because this diagnosis should only be given after everything else is ruled out. This is not the case, however.
Doctors should do a much better job at ruling out conditions before offering a fibromyalgia diagnosis. They need to consider all similar diseases or disorders first.
Keep reading to find out the more common conditions that mimic the symptoms of fibromyalgia.
1.Hypothyroidism
When your thyroid does not produce enough hormones, it is underactive, or hypothyroid.
Because so much of your body’s functions depends on proper functioning of the thyroid, when it is not working correctly, you will notice negative symptoms. Many of these symptoms are like those of fibromyalgia.
An underactive thyroid can hinder digestive functioning, as well as cause pain in your arms and legs. It can make you overly sensitive to temperature changes and bright lights. It has also been associated with depression and anxiety.
2. Rheumatoid Arthritis
Rheumatoid arthritis occurs when your immune system starts attacking the linings of your joints. This causes inflammation and severe pain in your joints. This disorder can affect every body part from your eyes, skin and blood, to your hands and feet.
You can expect to feel stiffness, extreme fatigue, and even fever.
And all these symptoms can lead to:
- Sleep problems
- Digestive issues
- Anxiety and depression
3. Lupus
Lupus is another autoimmune disease in which the immune system attacks its own tissues and organs. This can cause great pain all over the body. It can even hurt when you breathe. The muscles, bones, joints and skin are all effected.
- Inflammation
- Swelling
- Rashes
- Fatigue
- Swelling
- Severe pain
It can even produce sores and ulcers in your mouth and on other parts of the body.
Due to these symptoms, many sufferers feel anxious or depressed, and note they have a hard time sleeping and eating.
4. Lyme’s Disease
Lyme’s disease is caused by a bacterium. There are four types of bacteria that can lead to Lyme’s. Many doctors do not test for all four types when they should to eliminate it completely.
Lyme’s disease can cause severe headaches and neck stiffness. It causes rashes and inflammation in various parts of the body. Joint pain, muscle weakness and flu-like symptoms are presented with this disorder.
Extreme fatigue is often a common symptom among sufferers. As you can see, this is just one more condition that mimics fibromyalgia.
It can be quite concerning to think doctors are misdiagnosing diseases when there are many ways to avoid a fibromyalgia misdiagnosis.
How to Avoid a Fibromyalgia Misdiagnosis
There are things you can do to ensure you do not receive a fibromyalgia misdiagnosis. One of the first steps is finding the right doctor.
It’s important you do extensive research when seeking a doctor. The doctor you choose needs to have, at a minimum, extensive experience working in the field of pain medicine. They should be certified and licensed in the pain management.
Your doctor should have a variety of methods to use when diagnosing your symptoms. He or she should spend much time eliminating other conditions before giving you a diagnosis of fibromyalgia.
When treating your symptoms, your doctor should offer the best, most up-to-date options. They should be using current and cutting-edge techniques. A doctor that only wants to prescribe pain medicine is not the doctor for you.
Instead, your doctor should compliment your treatments with alternative or holistic therapies. They understand the mind, body and spirit are connected and should be treated together.
Conclusion
An organization that is seen as a positive model in treating patients with pain is the Comprehensive Pain Management Center. Finding out the cause of your pain is the first goal. Once the cause is determined, the right treatment can begin.
Make sure your doctor looks at every possible cause, and there are hundreds, of pain. They should never rush to a diagnosis, especially when there are so many tests and procedures at their disposal to help with diagnosing conditions.
The best doctors still need help from you. Make sure you report all symptoms, give detailed descriptions of when and where you have pain.
The more information you can offer, the easier it will be for the doctor to properly diagnose your pain.
Understanding Chronic Pain in Children & How to to Counter It

Chronic pain in children and teenagers is becoming more common, and is often not diagnosed for years. Here is how we can reduce the most common types of chronic pain children suffer from.
Reports have stated chronic pain in children is underdiagnosed and not treated properly in both children and teenagers.
Especially true are cases that deal with abdominal pains, musculoskeletal issues, joint pain and headaches.
Statistics have shown that up to 38 percent of children and adolescents have faced some type of chronic pain.
This number is frightening because eventually, these children and adolescents will be adults with chronic pain. That is, unless they are treated properly from the beginning.
Defining chronic pain in children is a great first step to understanding this epidemic and how to counter it.
What is Chronic Pain in Children?
An official definition of chronic pain in children came from the American Pain Society on Pediatric Chronic Pain.
They label it as: recurrent and consistent pain that lasts longer than it should, longer than normal healing times, often longer than three to six months.
The pain can be continuous or come and go, and can be different for each child.
The most common types of chronic pain in children include:
- Tension and migraine headaches
- Abdominal pain
- Growing pains
Main causes of chronic pain in children include:
- Tissue damage
- Nerve damage
- A problem with the nervous system
How Does Chronic Pain Affect Children?
Chronic pain can impact all areas of a child’s life. It can affect their mental and physical health, as well as socialization.
Chronic pain can lead to:
- Anxiety and depression
- Sleep problems
- An inability to concentrate
All of these can lead to poor performance in school and extra-curricular activities.
Children with chronic pain need a team of providers to help treat their issues so they can have a high quality of life. From a thorough and proper diagnosis to ongoing treatments, children need a full range of specialists.
Treatments can include all of the following:
- Medication
- Physical therapy
- Psychological counseling
- Specialized treatments provided by doctors at a pain management clinic
Below, we discuss some of the most common conditions of chronic pain in children, as well as what a pain management doctor can do to help counter the symptoms of pain.
1. Juvenile arthritis
Juvenile arthritis is diagnosed in children ages sixteen or younger who have experienced joint swelling and pain for more than six weeks, with no resolution.
This problem affects approximately 50,000 American children.
It is sometimes classified as rheumatoid arthritis or idiopathic arthritis in juveniles.
The inflammation associated with juvenile arthritis can be painful for a child. Their immune system does not work correctly.
It thinks some of the child’s tissues are foreign and therefore, tries to attack them, leading to
- Redness
- Swelling
- Stiffness
- Other symptoms of pain
Treatment Options
Treating juvenile arthritis is best with a pain management specialist. They can determine if the child requires anti-inflammatory drugs.
They can also obtain the right blood tests and x-rays to help form a treatment plan.
Corticosteroids may help some children combat the pain. Others may benefit from physical or occupational therapy, and in severe cases, surgery.
2. Complex Regional Pain Syndrome in Children
According to an online pediatric journal, musculoskeletal pain is a top reason children are referred to a doctor when it comes to pain they are experiencing.
Most experience
- Pain in their limbs
- Increased sensitivity in certain body part
- Temperature changes in affected areas
- Skin changes
- Limited range of motion
This issue is sometimes caused by injury to an area of the child’s body. However, this is not always the case.
That’s why working with a specialist is important in getting the right diagnosis and treatment.
Treatment Options
Treatments can include medications to reduce the pain, as well as steroids and bone protectors.
In addition, nerve blocking medicines may help as well.
Specialists may even determine the use of spinal cord stimulation; biofeedback, physical therapy and electrical nerve stimulation can be of benefit.
3. Fibromyalgia in Children
Sometimes referred to as juvenile primary fibromyalgia syndrome, a child can experience many negative symptoms. These include:
- Fatigue
- Soreness
- Headaches
- And can affect all areas of the body – a child’s tissues, muscles and joints can feel pain with this condition.
Some kids may have irritable bowel syndrome as a symptom, while others may have anxiety, depression and an inability to concentrate.
These can all become more severe if not treated properly.
Treatment Options
Exercise and physical therapy can help some children by stretching the muscles and learning how to relax the muscles.
Other therapies include medications such as steroids and anti-inflammatories.
Pain management specialists can help your child identify lifestyle triggers to avoid for preventative measures.
When unable to prevent symptoms, hot and cold treatments can be used, as well as alternative therapies such as massage, yoga, and meditation.
4. Headaches in Children
The reasons children get headaches can be broad.
- Some may be feeling overwhelmed and stressed.
- Others may be dehydrated.
- Their diet and the amount of sleep they get can also lead to headaches in children.
Vision problems, as well as a family history of headaches can also be causes of headaches.
Getting a proper diagnosis to find out the true source of your child’s headaches is important.
Once you find out the cause, your doctor can establish proper treatments.
Treatment Options
If your child is dealing with a chronic pain condition, a pain management specialist can develop specific therapies that may help.
Therapies can include vitamin infusions, hydration solutions and even stress relieving activities.
Your doctor may want to treat nutritional deficiencies to combat headaches, such as raising magnesium or iron levels.
In severe cases, anti-inflammatory medications may be useful. They can offer both abortive and preventative treatments to help relieve pain symptoms associated with headaches.
In addition, treatment involving chiropractic care, massage, cognitive behavioral therapy, and medical foods has been found to ease headaches in children.
Take the First Step
Chronic pain in children is much more common than one might think.
If your child is suffering from any type of pain, the first thing you can do is contact a pain management specialist who can give you a complete evaluation, diagnosis and will develop a plan that will help your child get back to living pain free.
Comprehensive Pain Management Center provides treatment for a variety of pain conditions. If you or a loved one is suffering from pain, contact us today.
Tingling Feet or Hands… Is It Peripheral Neuropathy?

You may have peripheral neuropathy if you are experiencing uncomfortable sensations in parts of your body.
If you have tingling in your feet or hands, burning sensations in your back or face, or muscle weakness or lack of coordination – it’s time to learn more.
If you are wondering what it is and how can you get rid of it, the first thing you need to do is visit a medical professional. This will allow for you to get an accurate diagnosis based on a thorough examination of your symptoms, including lab work and diagnostics. Your doctor may discover you have peripheral neuropathy.
What Is Peripheral Neuropathy?
When you hear the word shingles, or carpal tunnel syndrome, you may automatically grimace because you know (or know someone) who has experienced this pain. These are great examples of peripheral neuropathy.
Every person has a central nervous system and a peripheral nervous system.
The peripheral nervous system includes the brain and spinal cord, which are connected to nerves that send messages to the rest of your body like your:
- Arms
- Feet
- Legs
- Skin
- Muscles
When your nerves are damaged in any way, and the brain and spinal cord are unable to send messages to the rest of your body, this is called peripheral neuropathy.
Negative symptoms may become recognizable in the areas that need to get a message but can’t.
Negative symptoms can include:
- Tingling
- Stinging
- Burning
- Numbness
- Any other sensation that is uncomfortable, maybe even painful
Symptoms can be noticed in one or multiple areas of the body.
If this sounds familiar you may be wondering what causes peripheral neuropathy in the first place.
Causes of Peripheral Neuropathy
There can be many different reasons for damage in the peripheral nervous system, thus causing peripheral neuropathy.
- You may experience a trauma of some kind, like a car accident, in which you injure your nerve and could not make a full recovery.
- You may have an autoimmune disorder that has been known to be connected with peripheral neuropathy. Diabetes is a common cause of peripheral neuropathy. In fact, one report states that at least half of those diagnosed with diabetes also experienced symptoms related to nerve damage.
- Other reasons for this disorder include
- Alcoholism
- Infections
- Allergies
- Tumors
- Disorders of other vital organs such as the liver, kidney or even your thyroid
Genetics can even play a role in the development of peripheral neuropathy. All of which can lead to varying symptoms.
Symptoms of Peripheral Neuropathy
There is not a common symptom for every person suffering from peripheral neuropathy. Each case is individualized and symptoms vary based on the job the damaged nerve was supposed to be able to do.
If you are having muscle problems, you may receive symptoms of weakness, spasms or pain. This means your muscles are not receiving the messages it needs from your brain or spinal cord.
You may notice you are having difficulty picking up things, or that to touch something creates pain.
Sensory Symptoms
If so, peripheral neuropathy may be related to your sensory nerves. Damage to the sensory nerves may affect your
- Touch
- Sight
- Smell
- Hearing
- Taste
Other Symptoms
If there is damage to your motor senses, you may find it hard to balance yourself, walk on your own, or control your muscles. Muscle weakness and cramps are other symptoms.
Your automatic nerves send and receive messages related to body temperature, digestion, and blood pressure. So, if any of these are disrupted or painful, peripheral neuropathy may be the reason. Other symptoms can include
- Excessive sweating
- Dizziness
- Difficulty controlling your bladder
Don’t let these symptoms scare you. There is help. Treatment can work.
Getting Treatment
Treatment for peripheral neuropathy is individualized. This i just like the symptoms and causes. The best thing you can do is find a quality pain management center with medical professionals who have extensive knowledge and experience with this disorder.
A good pain management center will not just prescribe medication. Their goal is to reverse the problems in the area causing the nerve problems.
To do so, they will treat the whole body to ensure the connection between your mind and body is given the attention it needs to help you overcome peripheral neuropathy.
Working with your doctor, you will discover the root cause of your pain. From this point, you develop a treatment plan. Your treatment may include several different treatments.
There is rarely just one treatment procedure to deal with peripheral neuropathy.
Treatment Possibilities
Because pain can have an effect on both your mental and physical health, it is important you work with a doctor who prescribes techniques for improving both.
Options your doctor may pursue include anti-depressants, over the counter anti-inflammatory medicine, or prescription medication.
Other options include surgery and nerve stimulation or modulation therapies. Furthermore, your doctor should focus on your lifestyle and areas that may need improvement, such as diet and exercise. He or she will evaluate your nutrient levels and if you are lacking, may prescribe vitamins and minerals.
Therapies
Complementary treatment therapies may also include:
- Injections
- Massage therapy
- Acupuncture
- Medical food supplementation
- Exercise programs
There may even be a time where surgery is the answer. That is a decision for you and your doctor to make.
There are some up and coming alternative therapies to rid your body of toxins that can cause neuropathy.
One such treatment is Chelation Therapy, where you are giving a binding agent that connects to the toxins in your body so they can exit your body through your urine.
For immune disorders, Intravenous Immunoglobulin Therapy works to try and stop the immune process that is creating the damage in the first place.
Physical therapy is also available at some pain doctors to help treat muscles in pain from nerve damage.
Conclusion
Do not wait to seek treatment. There is a high likelihood your doctor can successfully treat your nerve issues.
Start the process today by reaching out to a pain management specialist. They are ready to help you live a pain free life.
5 Reasons to Visit Complex Regional Pain Syndrome Specialists

CRPS is a difficult, painful, and confusing type of chronic pain. During this difficult time, complex regional pain syndrome specialists can help.
If you are dealing with pain of any kind, your goal is to eliminate that pain as soon as possible.
You may have tried many options on your own, from over the counter pain remedies to alternative therapies to visiting your family doctor.
With each visit to your doctor, you may receive a different diagnosis or a different avenue to try for pain relief.
Some of these efforts may have even paid off temporarily. But after a while, you notice the pain returning.
This may be the perfect time to visit Complex regional pain syndrome specialists (CRPSS) in your area.
How Complex Regional Pain Syndrome Specialists Can Help
You want the most qualified person helping you find solutions to your pain problem.
That is exactly what complex regional pain syndrome specialists are: a person with years of education and experience researching and learning how to help patients cope with pain that is not easily defined.
You may be hesitant to visit a specialist at first.
However, there are at least five reasons meeting with a specialist can benefit you in your search for pain relief.
1. They Know the Most About Complex Regional Pain
Becoming complex regional pain specialists does not happen right after someone completes medical school.
In fact, it takes completion of medical school, specialty studies and residencies before one can become a CRPS pain specialist.
If you have chronic pain, you want someone who is a master in the area of treating chronic pain.
Just like if you were pregnant you want to seek treatment from an obstetrician and if you have a broken leg, you want to seek help from an orthopedic.
You want to work with the professional who can not only diagnose you properly but explain exactly what CRPS is in a way that is easy to understand.
2. They Can Explain CRPS To You
Compelx regional pain syndrome specialists can:
- Teach you about the diagnosis
- Explore and explain why you may have it
- Tell you how they plan to help you treat it
CRPS is simply pain experienced in the arms, hands, elbows, knees and legs areas. It is pain that makes those areas very sensitive.
Unfortunately, the pain source is not always easy to identify. But specialists can distinguish if the pain is coming from a previous injury or if it is related to nerve damage.
For most people, CRPS is chronic and can vary in degree of pain. It can even change the temperature and color of the skin in the pain area.
The specialist can tell you how he or she plans to treat your CRPS.
It is rare a specialist will just give you medicines and send you home.
They are more focused on healing you rather than just treating your symptoms.
3. They Treat Your Whole Mental and Physical Being
Because CRPS can originate in multiple locations, including the nervous system, complex regional pain syndrome specialists find it beneficial to treat all of you, mentally and physically.
They know that mental health is connected to physical health and treating both at the same time can lead to positive results.
Chronic pain has been associated with depression and anxiety in many people.
It’s true, when you feel bad physically it is hard to be happy and cheery at the same time.
Pain makes you feel bad and if you feel bad long enough, your mental health can be affected.
Just the opposite can be true also, with many studies recognizing that those diagnosed with mental illness such as depression have noted also having aches and pains with no specific source.
This leads researchers to believe depression can cause unwanted pains.
Your doctor can’t treat your whole body alone. Instead, they use a team of professionals.
4. Use the Help of a Team of Specialists
Treating CRPS by treating the whole body is key to long-term relief.
Leading a healthy lifestyle, as well as practicing mindfulness can help in treating your pain.
Complex regional pain syndrome specialists know there are other treatment providers who can assist them in helping you overcome your CRPS.
Stimulation
Spinal cord stimulation is one way.
In this treatment, and electrical device, like a pacemaker, is placed under the skin and for several days, the nerves of the spinal cord are stimulated.
If you experience less pain during the trial period, you will likely be recommended to have a small pulse generator can be implanted into your body and is set to send signals to your body that help alleviate pain.
Mental Health Specialists
In addition to a spinal cord stimulation specialist, you will also be treated by a mental health provider or counselor.
They can address any mental health obstacles that may be contributing to your pain.
Physical Therapists
Physical therapy has been shown to help ease chronic pain when used in combination with other treatments.
Other Treatment Specialists
Other team members may include acupressure and acupuncture therapists, massage therapists and even naturopaths who can introduce you to vitamins and supplements for better health.
Utilizing all these therapies can help you better manage pain in times of unexpected flare ups.
They can also offer you additional tips on how to handle your chronic pain, on your own, in between sessions with your treatment providers.
5. They Provide Additional Tips for Managing Pain
It may be tempting to take an opioid when your pain becomes unmanageable. But in some cases, it may be too late.
Meaning, a single dose of your medicine may not be enough to alleviate all the pain. This is when it is most important to have additional tips for managing pain.
Your CRPS specialist can offer tips and teach you new trends they have learned within the industry.
Tips may range from taking a hot or cold bath to joining a group with others who also suffer with CRPS.
The main tip is for you to be in control of your pain management and to not allow your pain to be in charge.
Working with complex regional pain syndrome specialists can help you gain the control you need to live with and hopefully overcome your pain.
Pain Awareness Month: Common Conditions and Treatments to Know
September is Pain Awareness Month from the American Chronic Pain Association. So this Pain Awareness Month, we want to share insight into the devastating condition and explore the most common conditions and treatments of chronic pain.
Are you one of the 76 million Americans living with chronic pain? If so, you are probably wondering if you will ever be able to find the right treatment.
This is a question many have, and the answer varies for each person. Pain comes from so many different sources in the body. However, a pain doctor can help you learn the different types of pain, and possible treatment options.
What Is Pain Awareness Month?
The goal of Pain Awareness Month is to raise public awareness of pain and pain management.
Pain management can be a difficult subject, which is why this Pain Awareness Month, all of us at Comprehensive Pain Management Center are striving to help inform the public of chronic pain.
Since everyone responds to pain differently, your doctor will need to help you create a personalized plan directed towards you.
The right pain doctor can evaluate your specific issues and form a diagnosis. From there, the two of you can create a treatment plan for management of your pain.
One of the first steps your doctor may take is determining if your pain is acute or chronic.
Acute Pain Vs Chronic Pain
Pain can be a good thing. It is like a defense mechanism, telling us what to stay away from, like a hot stove that can burn us if we touch it. Pain tells you what not to do to avoid being harmed.
Most of the time, pain is the result of an injury and is acute.
Stubbing your toe, hitting your head, or jamming your finger are examples of minor injury related pains. Breaking bones and damaging nerves can lead to deeper pain. However, once the injury heals, the pain usually subsides.
There are other times when the pain does not go away and becomes chronic. When you have chronic pain, your body is processing pain messages differently because your nervous system has altered how you perceive pain. It makes you much more sensitive to pain.
Sometimes even just a small bump or prick can feel unbearable.
Working with a pain doctor can help.
Below are some of the most common pain conditions and the treatments available to help ease your pain.
1. Back Pain
According to reports, lower back pain is the leading cause of disability worldwide. Back pain can affect your range of motion and can radiate pain upward and even down your arms and legs.
You may even feel other symptoms like tingling and numbness.
Treatment Options
Pain doctors are offering promising treatments to help patients with lower back pain. Sometimes pain treatment includes medicine and physical therapy.
Other times a patient may require steroid injections, spinal fusions, or surgery to remove damaged tissues.
Alternative treatments are great supplements to traditional methods. These may include yoga, massage therapy, acupuncture or acupressure.
If you’re suffering from back pain, contact us today to learn about the different treatment options you have.
2. Headaches
Everyone gets a headache occasionally. Some people can take aspirin and relieve their headache pain. Others, however, are unable to get rid of their headaches despite trying multiple treatments.
Headaches can be caused by many factors, from the eyes to neck or back tension to more serious injuries or dysfunctions. They are categorized as being either tension, migraine or cluster headaches.
Migraines effect one in seven people, according to the World Health Organization, with most sufferers between the ages of 35 and 45.
Pain management doctors can work with you to figure out the root source of your headaches. Then, they can begin a treatment plan to heal the source which will then alleviate the pain from the headaches.
Treatment Options
Treatment options used successfully by pain doctors include abortive and preventative therapies. The goal of abortive therapies for headaches is to stop the pain caused by the headache. Medicines such as ibuprofen, aspirin, oxygen, triptans and opiates can be one source of relief.
Other techniques may involve the use of steroids or lidocaine.
Preventative therapies help to decrease the number of headaches you have, as well as the pain and disability that appear with your headaches. Your pain doctor may prescribe anti-seizure medication, antidepressants, and even Botox to manage your headaches more effectively.
3. Joint Pain
If you have had an injury, infection or are just experiencing signs of aging, chronic joint pain can make it difficult to function. Ordinary daily tasks can feel excruciating.
Arthritis is the most common type of joint pain experienced by Americans, with some reports showing one out of every two people have some form of arthritis.
These can include osteoarthritis, rheumatoid arthritis, bursitis, and tendinitis.
Treatment Options
Treatment options for pains associated with the joints can range from exercise to steroid injections. Medial branch blocks have shown to reduce inflammation among patients. If severe and persistent for lengthy periods, replacing the joints may be a viable option.
4. Nerve Pain
When a nerve is damaged, it can be very painful. There are many reasons for nerve pain. Your nerve may have been compressed, as with sciatica, and can send shooting pains down your legs. Or, you may have pain due to repetitive motions, like with carpal tunnel syndrome.
Treatment Options
In some cases, medications can break down the myelin sheath. Meaning, your nerves are no longer protected, leaving them exposed to elements that can cause pain.
Specialized treatments for nerve pain can range from taking anti-inflammatory drugs to electrical stimulation to trigger point injections. Some patients find relief with infusion techniques, while others prefer disc decompression.
The Importance of a Pain Management Doctor
You and your pain doctor, after a comprehensive exam, will develop the right treatment plan for your pain. Treatment can include both holistic and traditional methods, incorporating several techniques to address your nerve pain.
Pain can interfere with your daily activities, and even relationships. It can make it hard for you to complete ordinary tasks at work and home.
You deserve to live a life that is pain free, or at least manageable so you can live a quality lifestyle. Don’t wait any longer to choose a pain doctor who can help you with your pain.
This Pain Awareness Month, look for a doctor who listens to you, and assesses your situation using many tools and techniques to get a good overall evaluation.
A good pain doctor is one who teaches you why you are in pain rather than just giving you a prescription. It’s important for you to understand your body, why it is experiencing pain, and what you can do to make the situation better.
Together, you and your pain doctor can help you reach success in coping with your pain.
What Is Causing My Radiating Leg Pain?

Radiating leg pain means you are hurting in one place on the body that is also causing pain to move to other parts, such as your leg. For instance, you may have a back problem that causes referred pain in your legs.
All pain can be troublesome. But when it radiates to other places on your body, it can feel overwhelming.
Radiating leg pain is more common than you may think, and many times comes from an ailment in the back, spine or some place other than your actual leg.
The best way to treat your leg pain is to work with your doctor in finding the root of the problem.
You need to discover the starting point of the pain, so you can then find out why the pain moves to your legs.
Identify Exact Symptoms of Radiating Leg Pain
To help your doctor determine what is causing your leg pain, it’s important you describe your symptoms accurately.
Your doctor is not able to feel your pain, so they need to hear from you exactly what you are feeling and where.
When describing your leg pain, be able to tell the doctor if you feel a burning sensation, weakness, numbing, tingling, or heaviness.
Is it a constant pain or come and go depending on whether you are moving or sitting still?
Tell your doctor if the pain starts in one location and moves to another, or if it starts and stops in the same place in your leg.
Tell them if it feels painful on the inside or outside of your leg.
In addition, inform your doctor of the location on your leg that is in pain.
Radiating leg pain can create agitation in the front or back thigh muscles, knees, shins, the calf, your toes, and even your groin.
Tell them every specific detail you can about your symptoms, so they can make an accurate diagnosis.
Risk Categories of Pain
Your doctor will assess the category in which your pain falls.
These categories help them determine probable causes of your leg pain.
The categories include low-risk, low-medium-risk, medium-risk, medium-high-risk, and high-risk.
Low-risk pain refers to pain that is easily manageable. You may find taking over the counter medications like ibuprofen ease the pain. Or, avoiding use of the area in pain helps you feel relief.
Low-medium-risk is pain that needs to be managed by a prescription medication, while medium-risk may require a more emergent visit to your doctor or hospitalization.
Medium-high-risk means you have a problem that is urgent and needs immediate attention. You may go to an emergency room for help relieving the pain. While the pain is not life threatening, it can feel as if it is.
High-risk, on the other hand, is life threatening and may even require intensive care in a hospital environment.
Common Sources of Pain Associated with Risk Category
Pain determined to be of high-risk are sometimes associated with major organ malfunction, such as kidney failure or infections.
When the organs are not working properly, other body parts, such as the legs, can feel pain.
Bone cancer, or other types of cancers, can also create radiating pain.
There is a connection between diabetes and leg pain. Any pain of this type is critical and should be hospitalized for treatment.
Medium-risk types of pain are most often associated with pinched nerves, inflammation, herniated discs, fractured vertebrae, muscle tears, spinal or disc infections, and even tumors.
It’s important to seek advanced medical treatment immediately to avoid further damage and more intense pain.
While not life threatening, these causes of pain can become worse over time.
Lower-risk causes of pain can be related to the sciatic nerve, pulled hamstring muscle, pulled muscles in the back and arthritis, to name a few.
Other Sources of Radiating Leg Pain
Does your pain get worse when you are moving around, like walking or running?
This should be discussed with your doctor.
There are types of radiating pains that happen while moving, and there are pains that occur when you are still.
Even worse, there are pains that take place whether you are still or moving.
An example of a pain that happens when you are moving around could be the result of your blood vessels being in distress.
This problem can result in blood clots or deep vein thrombosis.
When you have been inactive for a while, and if blood supply is not circulating in your legs properly, a blood clot can develop. This can be very painful.
Neuropathy happens when the nerves in the spinal system that connect to muscles or organs become dysfunctional.
The result is numbing, tingling feelings and even lack of feeling at all in the legs.
Furthermore, radiating leg pain can appear when there is a lack of electrolytes in the body.
Meaning, your body is not receiving important minerals and vitamins such as potassium and calcium needed for proper functioning.
Arthritis and back injuries or diseases are also known to cause radiating leg pain.
Getting Help
The steps involved in relieving your pain begin with obtaining an accurate diagnosis from your doctor. To do this, your doctor should give you a physical exam, as well as utilizing x-rays and other testing such as MRIs.
The diagnosis will also be made through an analysis of the fluids in your areas of pain when necessary.
Doctors will also use the process of exclusion of other diseases to help determine the cause of your pain.
Treatments for your pain will depend on the level of severity.
A minor injury can be prescribed a rotation of heat and ice, with over the counter analgesics.
On the other hand, severe cases can involve surgeries and pain management for any chronic symptoms.
The best thing you can do to get to the root of your radiating leg pain is to be honest with your physician about your symptoms, how long you have experienced pain, and any potential reasons for the pain.
Allow your doctor to conduct all the tests they need to provide you with an effective treatment plan.
Your doctor’s goal is the same as yours, to relieve your pain as soon as possible.
The Best Pain Management Treatment Options

Back pain can disrupt your lifestyle. Whether your pain is muscular, skeletal or unknown, it can control how well you function in everyday activities. Severe back pain can make it hard to walk or complete ordinary tasks. However, different pain management treatment options can increase your quality of day to day life by healing your pain.
Often, pain in your back can lead to pain in other places in your body. Back pain can shoot to your legs, neck and even arms. Some people note they experience migraines on top of the pain they feel in their back. In addition, pain can range from achy and dull to stinging or burning.
Some may feel a numbing or tingling, while others may feel spasms and tightness. Some people may have back pain for a few days or weeks, while others may experience chronic pain that lasts for months.
Back pain is truly unique to the individual.
Types of Back Pain
Generally, there are two common types of back pain. Mechanical back pain refers to pain that originates from the muscles, joints, ligaments or bones surrounding the spine. Depending on how you sit, walk, and move around, the pain can increase or decrease.
Radicular pain deals more with the nerves of the spine, when they become pinched or inflamed. The pain is typically sharp and burning, shooting down through the legs.
Back pain can also come from other parts of the body that may be suffering an injury or abnormality. Kidney stones is an example of this.
Getting the right diagnosis for your back pain is the first, and most important, step in developing a pain management treatment plan.
Getting a Diagnosis for Back Pain
Proper diagnosis begins with a comprehensive evaluation by qualified medical professionals, ones that specialize in the treatment of back pain.
The goal of health professionals should be to increase your ability to function, while decreasing your pain symptoms.
Ultimately, they should try to heal your pain through cutting edge treatments, mixed with therapies and other techniques.
In some cases, when a source of pain cannot be eliminated, the symptoms can still be reduced.
Quality pain doctors will provide you with extensive education regarding your source of pain, as well as information on all treatment options available. Keep reading to learn more on common treatment options.
Conservative Pain Management Treatment Options for Back Pain
Doctors will likely start with more conservative treatment options to alleviate your back pain. Conservative treatments include taking aspirin or ibuprofen. Other conservative methods may include physical therapy, nerve pain relievers, and simply allowing time to heal wounds.
Rest and relaxation can sometimes be the best prescription. Controlled substances are used after more conservative options fail. Doctors also implement other treatment methods such as steroid injections.
Steroid Injections for Back Pain
Steroid injections relieve pain in the lower back and legs. Pain may be originating from inflammation or herniated discs. Steroid shots are not the first measure a doctor will explore but if treatments like ibuprofen do not work, doctors turn to steroid injections.
Steroid shots include numbing agents as well as anti-inflammatory medicines, giving you relief from pain in target areas.
Some target areas are more common than others. For instance, epidural injections target nerve areas at the roots that extend to other areas of the body. Tendons, or inflammation of tendons, is another common target area.
Arthritis is a problem suffered by many. Steroid injections inserted into joints can calm inflammation associated with arthritis.
Spinal Cord Simulator Implant for Back Pain
The spinal cord stimulator implant takes advantages of electrical impulses that prevent pain signals from being sent to the brain. The remarkable thing about this device is that the patient or the doctor can use it as needed.
Doctors use these implants on patients who no longer benefit from conservative pain management treatment techniques.
Most patients undergo a trial period first and if the device works, the implant is put in later with a more permanent device.
The implant is controlled externally and can be adjusted as you see fit, increasing or decreasing the amount of stimulation to send.
Celiac Plexus Block Procedure for Back Pain
The celiac plexus is comprised of a bunch of nerves surrounding the aorta. This procedure, however, is set up to eliminate pain in the abdomen.
Because the celiac plexus leads to the abdomen, blocking these nerves will prevent pain signals from entering the abdomen.
If you have chronic pain in your abdomen, pancreatitis, or any cancers of the pancreas, the celiac plexus block procedure could benefit you.
Superion Indirect Decompression System for Back Pain
The superion indirect decompression system is primarily used on those who suffer from lumbar spinal stenosis (LSS), which is a degenerative condition of the spine. It refers to the wear and tear, or aging, of the spine over time. LSS can cause narrowing of the spine, which creates a pinching of the nerves in the back.
The superion indirect decompression system basically opens the spinal canal so the nerves are no longer pinched.
Back Pain Management Treatment Using Disc Denervation
Pain associated with the facet joint is quite commonly chronic for those with neck and back pain. Disc denervation is a good pain management treatment option by using such things as radio frequency ablation. It gets rid of abnormal tissue with the use of extreme levels of heat through electrical stimulation.
There is specific information you can give your pain management treatment doctor that will help in your diagnosis. You may find taking notes on your pain to give to your doctor can help.
Providing answers to the following questions can help your doctor visualize and understand your pain:
- Where is the pain?
- Does it stay in the same place or relocate?
- Does your pain ease or get worse depending on how you are standing or sitting?
- Other than pain, do you have other sensations like tingling or numbing?
- How has your pain affected your quality of life?
- How has your pain affected others in your life such as family and friends?
From there, your doctor will be able to choose the right pain management treatment to help you feel better as quickly as possible.